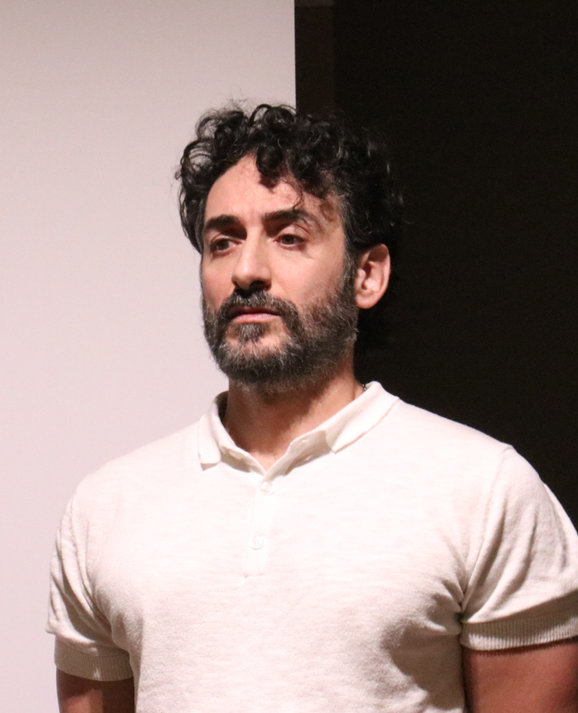
Roberto Di Gesù
@fondazionerimed.eu
Principal Investigator, Musculoskeletal Tissue Engineering (MsTE) lab.
Ri.MED foundation
I am the principal investigator of the musculoskeletal tissue engineering lab. at Foundation, a biomedical and biotechnology
center of excellence in Palermo, Italy. I have been a visiting research scientist at University of Pittsburgh and at Children's Hospital of Philadelphia, two of the top research institutions in the US. I initially graduated from Pharmacy School, then continued to complete my PhD in Biotechnology at University of Palermo working on bone tissue engineering and on drug delivery for cancer and Alzheimer's. During my first postdoc, I developed polymeric drug delivery systems (DDS) to treat maculopathy. Then I worked for two years as a senior scientist at Merck in Rome, developing an anti-cancer monoclonal antibody currently commercialized in the US as Bavencio. Then, I joined the University of Bologna working on electrospun DDS for spinal cord injuries. In I am engineering 3D in vitro models to study and treat musculoskeletal disorders.
EDUCATION
PhD, PharmD
RESEARCH, TEACHING, or OTHER INTERESTS
Biomedical Engineering, Biotechnology, Bioengineering
Scopus Publications
Scholar Citations
Scholar h-index
Scholar i10-index
Scopus Publications
R Di Gesù, A Palumbo Piccionello, G Vitale, S Buscemi, S Panzavolta, M F Di Filippo, A Leonarda, M Cuccia, A Di Prima, and R Gottardi
IOP Publishing
Abstract Osteoarthritis (OA) is a debilitating joint condition affecting millions of people worldwide, triggering painful chondral defects (CDs) that ultimately compromise the overarching patients’ quality of life. Currently, several reconstructive cartilage techniques (RCTs) (i.e.: matrix-assisted autologous chondrocytes implantation has been developed to overcome the total joint replacement limitations in the treatment of CDs. However, there is no consensus on the effectiveness of RCTs in the long term, as they do not provide adequate pro-regenerative stimuli to ensure complete CDs healing. In this study, we describe the biofabrication of an innovative scaffold capable to promote the CDs healing by delivering pro-regenerative hypoxic cues at the cellular/tissue level, to be used during RCTs. The scaffold is composed of a gelatin methacrylate (GelMA) matrix doped with hypoxic seeds of GelMA functionalized with a fluorinated oxadiazole (GelOXA), which ensures the delivery of hypoxic cues to human articular chondrocytes (hACs) embedded within the scaffold. We found that the GelMA/GelOXA scaffold preserved hACs viability, maintained their native phenotype, and significantly improved the production of type II collagen. Besides, we observed a reduction in type I and type X collagen, characteristic of unhealthy cartilage. These findings pave the way for the regeneration of healthy, hyaline-like cartilage, by delivering hypoxic cues even under normoxic conditions. Furthermore, the GelMA/GelOXA scaffold’s ability to deliver healing signals directly to the injury site holds great potential for treating OA and related CDs, and has the potential to revolutionize the field of cartilage repair and regenerative medicine.
Anna Liguori, Junwei Zhao, Roberto Di Gesù, Rossella De Marco, Chiara Gualandi, Natalia Calonghi, Antonino Pollicino, Luca Gentilucci, and Maria Letizia Focarete
Elsevier BV
Riccardo Bonsignore, Elisa Trippodo, Roberto Di Gesù, Anna Paola Carreca, Simona Rubino, Angelo Spinello, Alessio Terenzi, and Giampaolo Barone
Royal Society of Chemistry (RSC)
Novel DNA binding half Salphen cobalt(iii)complexes with promising anticancer activity on 3D cultured models.
Elisa Capuana, Davide Marino, Roberto Di Gesù, Vincenzo La Carrubba, Valerio Brucato, Rocky S. Tuan, and Riccardo Gottardi
S. Karger AG
Articular cartilage is crucially influenced by loading during development, health, and disease. However, our knowledge of the mechanical conditions that promote engineered cartilage maturation or tissue repair is still incomplete. Current in vitro models that allow precise control of the local mechanical environment have been dramatically limited by very low throughput, usually just a few specimens per experiment. To overcome this constraint, we have developed a new device for the high throughput compressive loading of tissue constructs: the High Throughput Mechanical Activator for Cartilage Engineering (HiT-MACE), which allows the mechanoactivation of 6 times more samples than current technologies. With HiT-MACE we were able to apply cyclic loads in the physiological (e.g., equivalent to walking and normal daily activity) and supra-physiological range (e.g., injurious impacts or extensive overloading) to up to 24 samples in one single run. In this report, we compared the early response of cartilage to physiological and supra-physiological mechanical loading to the response to IL-1β exposure, a common but rudimentary in vitro model of cartilage osteoarthritis. Physiological loading rapidly upregulated gene expression of anabolic markers along the TGF-β1 pathway. Notably, TGF-β1 or serum was not included in the medium. Supra-physiological loading caused a mild catabolic response while IL-1β exposure drove a rapid anabolic shift. This aligns well with recent findings suggesting that overloading is a more realistic and biomimetic model of cartilage degeneration. Taken together, these findings showed that the application of HiT-MACE allowed the use of larger number of samples to generate higher volume of data to effectively explore cartilage mechanobiology, which will enable the design of more effective repair and rehabilitation strategies for degenerative cartilage pathologies.
Irene Chiesa, Roberto Di Gesù, Kalon J. Overholt, and Riccardo Gottardi
Springer US
Mattia Pasqua, Roberto Di Gesù, Cinzia Maria Chinnici, Pier Giulio Conaldi, and Maria Giovanna Francipane
MDPI AG
The possibility to reproduce key tissue functions in vitro from induced pluripotent stem cells (iPSCs) is offering an incredible opportunity to gain better insight into biological mechanisms underlying development and disease, and a tool for the rapid screening of drug candidates. This review attempts to summarize recent strategies for specification of iPSCs towards hepatobiliary lineages —hepatocytes and cholangiocytes—and their use as platforms for disease modeling and drug testing. The application of different tissue-engineering methods to promote accurate and reliable readouts is discussed. Space is given to open questions, including to what extent these novel systems can be informative. Potential pathways for improvement are finally suggested.
Matteo Bulati, Rosalia Busà, Claudia Carcione, Gioacchin Iannolo, Giuseppina Di Mento, Nicola Cuscino, Roberto Di Gesù, Antonio Palumbo Piccionello, Silvestre Buscemi, Anna Paola Carreca,et al.
MDPI AG
Currently, Klebsiella pneumoniae is a pathogen of clinical relevance due to its plastic ability of acquiring resistance genes to multiple antibiotics. During K. pneumoniae infections, lipopolysaccharides (LPS) play an ambiguous role as they both activate immune responses but can also play a role in immune evasion. The LPS O2a and LPS O2afg serotypes are prevalent in most multidrug resistant K. pneumoniae strains. Thus, we sought to understand if those two particular LPS serotypes were involved in a mechanism of immune evasion. We have extracted LPS (serotypes O1, O2a and O2afg) from K. pneumoniae strains and, using human monocytes ex vivo, we assessed the ability of those LPS antigens to induce the production of pro-inflammatory cytokines and chemokines. We observed that, when human monocytes are incubated with LPS serotypes O1, O2a or O2afg strains, O2afg and, to a lesser extent, O2a but not O1 failed to elicit the production of pro-inflammatory cytokines and chemokines, which suggests a role in immune evasion. Our preliminary data also shows that nuclear translocation of NF-κB, a process which regulates an immune response against infections, occurs in monocytes incubated with LPS O1 and, to a smaller extent, with LPS O2a, but not with the LPS serotype O2afg. Our results indicate that multidrug resistant K. pneumoniae expressing LPS O2afg serotypes avoid an initial inflammatory immune response and, consequently, are able to systematically spread inside the host unharmed, which results in the several pathologies associated with this bacterium.
Riccardo Gottardi, Kim Moeller, Roberto Di Gesù, Rocky S. Tuan, Martijn van Griensven, and Elizabeth R. Balmayor
Frontiers Media SA
After surgical tendon repair, the tendon-to-bone enthesis often does not regenerate, which leads to high numbers of rupture recurrences. To remedy this, tissue engineering techniques are being pursued to strengthen the interface and improve regeneration. In this study, we used hyperelastic biphasic 3D printed PLGA scaffolds with aligned pores at the tendon side and random pores at the bone side to mimic the native insertion side. In an attempt to recreate the enthesis, the scaffolds were seeded with adult human mesenchymal stem cells and then cultured in dual fluidic bioreactors, which allows the separate in-flow of tenogenic and chondrogenic differentiation media. MTS assay confirmed the ability of cells to proliferate in dual-flow bioreactors at similar levels to tissue culture plate. Hematoxylin-eosin staining confirmed a compact cell layer entrapped within newly deposited extracellular matrix attached to the scaffolds’ fibers and between the porous cavities, that increased with culture time. After 7, 14, and 21 days, samples were collected and analyzed by qRT-PCR and GAG production. Cultured constructs in dual fluidic bioreactors differentiate regionally toward a tenogenic or chondrogenic fate dependent on exposure to the corresponding differentiation medium. SOX9 gene expression was upregulated (up to 50-fold compared to control) in both compartments, with a more marked upregulation in the cartilaginous portion of the scaffold, By day 21, the cartilage matrix marker, collage II, and the tendon specific marker, tenomodulin, were found to be highly upregulated in the cartilaginous and tendinous portions of the construct, respectively. In addition, GAG production in the treated constructs (serum-free) matched that in control constructs exposed to 10% fetal bovine serum, confirming the support of functional matrix formation in this system. In summary, our findings have validated this dual fluidic system as a potential platform to form the tendon enthesis, and will be optimized in future studies to achieve the fabrication of distinctly biphasic constructs.
Luisa Stella Dolci, Rosaria Carmela Perone, Roberto Di Gesù, Mallesh Kurakula, Chiara Gualandi, Elisa Zironi, Teresa Gazzotti, Maria Teresa Tondo, Giampiero Pagliuca, Natalia Gostynska,et al.
MDPI AG
Vascular and traumatic injuries of the central nervous system are recognized as global health priorities. A polypharmacology approach that is able to simultaneously target several injury factors by the combination of agents having synergistic effects appears to be promising. Herein, we designed a polymeric delivery system loaded with two drugs, ibuprofen (Ibu) and thyroid hormone triiodothyronine (T3) to in vitro release the suitable amount of the anti-inflammation and the remyelination drug. As a production method, electrospinning technology was used. First, Ibu-loaded micro (diameter circa 0.95–1.20 µm) and nano (diameter circa 0.70 µm) fibers were produced using poly(l-lactide) PLLA and PLGA with different lactide/glycolide ratios (50:50, 75:25, and 85:15) to select the most suitable polymer and fiber diameter. Based on the in vitro release results and in-house knowledge, PLLA nanofibers (mean diameter = 580 ± 120 nm) loaded with both Ibu and T3 were then successfully produced by a co-axial electrospinning technique. The in vitro release studies demonstrated that the final Ibu/T3 PLLA system extended the release of both drugs for 14 days, providing the target sustained release. Finally, studies in cell cultures (RAW macrophages and neural stem cell-derived oligodendrocyte precursor cells—OPCs) demonstrated the anti-inflammatory and promyelinating efficacy of the dual drug-loaded delivery platform.
Roberto Di Gesù, Abhinav P. Acharya, Ian Jacobs, and Riccardo Gottardi
Informa UK Limited
ABSTRACT Airway and other head and neck disorders affect hundreds of thousands of patients each year and most require surgical intervention. Among these, congenital deformity that affects newborns is particularly serious and can be life-threatening. In these cases, reconstructive surgery is resolutive but bears significant limitations, including the donor site morbidity and limited available tissue. In this context, tissue engineering represents a promising alternative approach for the surgical treatment of otolaryngologic disorders. In particular, 3D printing coupled with advanced imaging technologies offers the unique opportunity to reproduce the complex anatomy of native ear, nose, and throat, with its import in terms of functionality as well as aesthetics and the associated patient well-being. In this review, we provide a general overview of the main ear, nose and throat disorders and focus on the most recent scientific literature on 3D printing and bioprinting for their treatment.
Irene Chiesa, Carmelo De Maria, Anna Lapomarda, Gabriele Maria Fortunato, Francesca Montemurro, Roberto Di Gesù, Rocky S Tuan, Giovanni Vozzi, and Riccardo Gottardi
IOP Publishing
Abstract Bone is a highly vascularized tissue, in which vascularization and mineralization are concurrent processes during skeletal development. Indeed, both components should be included in any reliable and adherent in vitro model platform for the study of bone physiology and pathogenesis of skeletal disorders. To this end, we developed an in vitro vascularized bone model, using a gelatin-nanohydroxyapatite (gel-nHA) three-dimensional (3D) bioprinted scaffold. First, we seeded human mesenchymal stem cells (hMSCs) on the scaffold, which underwent osteogenic differentiation for 2 weeks. Then, we included lentiviral-GFP transfected human umbilical vein endothelial cells (HUVECs) within the 3D bioprinted scaffold macropores to form a capillary-like network during 2 more weeks of culture. We tested three experimental conditions: condition 1, bone constructs with HUVECs cultured in 1:1 osteogenic medium (OM): endothelial medium (EM); condition 2, bone constructs without HUVECs cultured in 1:1 OM:EM; condition 3: bone construct with HUVECs cultured in 1:1 growth medium:EM. All samples resulted in engineered bone matrix. In conditions 1 and 3, HUVECs formed tubular structures within the bone constructs, with the assembly of a complex capillary-like network visible by fluorescence microscopy in the live tissue and histology. CD31 immunostaining confirmed significant vascular lumen formation. Quantitative real-time PCR was used to quantify osteogenic differentiation and endothelial response. Alkaline phosphatase and runt-related transcription factor 2 upregulation confirmed early osteogenic commitment of hMSCs. Even when OM was removed under condition 3, we observed clear osteogenesis, which was notably accompanied by upregulation of osteopontin, vascular endothelial growth factor, and collagen type I. These findings indicate that we have successfully realized a bone model with robust vascularization in just 4 weeks of culture and we highlighted how the inclusion of endothelial cells more realistically supports osteogenesis. The approach reported here resulted in a biologically inspired in vitro model of bone vascularization, simulating de novo morphogenesis of capillary vessels occurring during tissue development.
Roberto Di Gesù, Chiara Gualandi, Andrea Zucchelli, Anna Liguori, Laura Paltrinieri, and Maria Letizia Focarete
Elsevier BV
R. Di Gesù, G. Amato, and R. Gottardi
Edra SpA
LEVEL OF EVIDENCE: 3 SUMMARY Tissue engineering (TE) is a growing scientific field that combine bioengineering, life science and clinical sciences. This scientific field represents a valid alternative to treatment of several diseases such as cardiovascular pathologies, osteoarthritis, skin burns, and different traumatic injuries. One of the most useful technique employed to produce valid scaffold for tissue engineering is the electrospinning, that allow to obtain highly customizable nanopatterned meshes. The aim of this review is to give an overview of the currently available literature on electrospun scaffold aimed to regenerate tendons and ligaments using a TE approach.
E. Campodoni, T. Patrício, M. Montesi, A. Tampieri, M. Sandri and S. Sprio
Elsevier
Roberto Di Gesù, Andrea Merlettini, Chiara Gualandi, and Maria Letizia Focarete
Elsevier
Roberto Di Gesù, Maria Luisa Bondì, Antonina Azzolina, Emanuela Fabiola Craparo, Chiara Botto, Erika Amore, Gaetano Giammona, and Melchiorre Cervello
Springer Science and Business Media LLC
Graziella Valenti, Stefania La Carta, Giovanni Mazzotti, Marco Rapisarda, Stefania Perna, Roberto Di Gesù, Loris Giorgini, Domenico Carmelo Carbone, Giuseppe Recca, and Paola Rizzarelli
Wiley
During last decades, implantable drug delivery systems (DDS) have been developed to optimize therapeutic properties of drugs and ensure their release in a specific site. Acrylic polymers have obtained growing interest in biomedical applications for their biocompatibility and chemical properties that make them extremely versatile. In this work, we focused on the realization of polymeric systems for controlled and sustained release of betamethasone 17,21‐dipropionate (BDP), a corticosteroid drug, in the treatment of the posterior eye diseases (PED). The investigated DDS were made of opportunely designed methacrylic block copolymers. Different series of methylmethacrylate/2‐hydroxyethylmethacrylate (MMA/HEMA) block copolymers, with various monomeric compositions (20‐60 mol% HEMA), were synthetized by Atom Transfer Radical Polymerization to find the best hydrophilic/hydrophobic ratio, able to ensure optimal kinetic release. Copolymers were characterized by nuclear magnectic resonance, size exclusion chromatography, and differential scanning calorimetry. Monitoring of drug release from films loaded with BDP was carried out by HPLC analysis. In particular, PMMA‐b‐PHEMA with 47 mol% of HEMA showed the best release profile to achieve the therapeutic reference dose, used in the treatment of PED (1‐3 µg/day), up to four months. Additionally, intraocular inserts with different shapes were prepared using silicon molds made by means of a 3D printer. POLYM. ENG. SCI., 57:570–578, 2017. © 2017 Society of Plastics Engineers
G. Valenti, S. La Carta, G. Mazzotti, M. Rapisarda, S. Perna, R. Di Gesù, L. Giorgini, D. Carbone, G. Recca, and P. Rizzarelli
Author(s)
Diseases affecting posterior eye segment, like macular edema, infection and neovascularization, may cause visual impairment. Traditional treatments, such as steroidal-drugs intravitreal injections, involve chronic course of therapy usually over a period of years. Moreover, they can require frequent administrations of drug in order to have an adequately disease control. This dramatically reduce patient’s compliance. Efforts have been made to develop implantable devices that offer an alternative therapeutic approach to bypass many challenges of conventional type of therapy. Implantable drug delivery systems (DDS) have been developed to optimize therapeutic properties of drugs and ensure their slow release in the specific site. Polymeric materials can play an essential role in modulating drug delivery and their use in such field has become indispensable. During last decades, acrylic polymers have obtained growing interest. Biocompatibility and chemical properties make them extremely versatile, allowing their...
Maria Bondì, Antonina Azzolina, Emanuela Craparo, Chiara Botto, Erika Amore, Gaetano Giammona, and Melchiorre Cervello
Springer Science and Business Media LLC
M. L. Bondì, E. F. Craparo, P. Picone, G. Giammona, R. Di Gesù, and M. Di Carlo
American Scientific Publishers
In this paper, the preparation, chemical-physical, technological and in vitro characterization of nanostructured lipid carriers (NLC) carrying R-flurbiprofen ester prodrugs, were analyzed for a potential pharmaceutical application. R-flurbiprofen was chosen as a model drug because it has been found to play an effective role in counteracting secretases involved in neurodegenerative diseases, although it does not cross the Blood Brain Barrier (BBB). In this study, two R-flurbiprofen ester prodrugs (ethyl and hexyl) were successfully synthesized and entrapped into non-pegylated and pegylated NLC. The obtained systems showed average diameters in the colloidal size range, negative zeta potential values and a good loading capacity. Drug release studies in physiological media on all drug-loaded samples showed a controlled drug release both at at pH 7.4 (containing esterase or not) and in human plasma of each ester prodrug, with a complete hydrolysis to R-flurbiprofen in media containing esterase. Empty and ethyl prodrug-loaded NLC were also demonstrated to have no cytotoxicity on human neuroblastoma (LAN5) cells, while hexyl prodrug-loaded NLC caused a reduction of cell viability probably due to a better capability of prodrug-loaded NLC to cross the cell membrane than the free compounds. These data were confirmed by microscopical observation, in which only the cells treated with hexyl prodrug-loaded NLC showed morphological changes. Outcoming data suggest that NLC could be potential carriers for parenteral administration of ethyl ester of R-flurbiprofen in the treatment of neurodegenerative diseases such as Alzheimer's.
Maria Luisa Bondì, Roberto Di Gesù, and Emanuela Fabiola Craparo
Elsevier
Maria Luisa Bondì, Montana, Bonura, Colombo, Emanuela Fabiola Craparo, Giammona, and Roberto di Gesù
Informa UK Limited
Parietaria pollen is one of the major causes of allergic reaction in southern Europe, affecting about 30% of all allergic patients in this area. Specific immunotherapy is the only treatment able to modify the natural outcome of the disease by restoring a normal immunity against allergens. The preparation of allergen-solid lipid nanoparticles as delivery vehicles for therapeutic proteins, P. judaica major allergen Par j 2, was investigated. The Par j 2 allergen was expressed in a large amount in Escherichia coli and purified to homogeneity. Its immunological properties were studied by western blotting and enzyme-linked immunosorbent assay inhibition. Solid lipid nanoparticles were obtained by water-in-oil-in-water multiple emulsion method and characterized in terms of mean size and surface charge. These systems (approximately 250 nm diameter and negative surface charge) incorporated recombinant Par j 2 with 40% or greater efficiency. Moreover, the endotoxin level and anaphylactic activity of the empty solid lipid nanoparticles and recombinant Par j 2-loaded solid lipid nanoparticles were evaluated by looking at the overexpression of CD203c marker on human basophils. These results demonstrate that recombinant Par j 2-nanoparticles could be proposed as safe compositions for the development of new therapeutic dosage forms to cure allergic reactions.
M. Bondì, E. Craparo, P. Picone, M. Carlo, R. Gesu, G. Capuano, and G. Giammona
Bentham Science Publishers Ltd.
Department of Electrical Engineering, Indian Institute of Technology, Kharagpur 721 302, India, Electrical Engineering Division, Engineering Department, University of Cambridge, 9 J.J. Thomson Avenue, Cambridge CB3 0FA, UK, Faculty of Electrical Engineering, Universiti Teknologi Malaysia, UTM Skudai 81310, Johor, Malaysia, Department of Physics, Indian Institute of Technology, Mumbai 400 076, India, Division of Engineering and Physics, Wilkes University, Wilkes-Barre, PA18707, USA