CORAUX Christelle
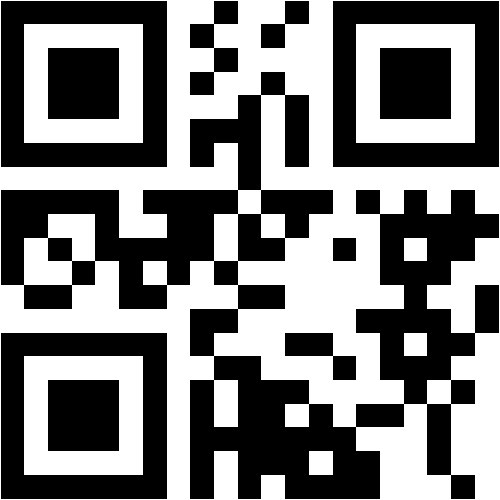
@univ-reims.fr
Scopus Publications
Scopus Publications
Manuella Lévêque, Sandra Mirval, Christine Barrault, Isabelle Fixe, Christelle Coraux, Edouard Sage, Frédéric Becq, and Clarisse Vandebrouck
Springer Science and Business Media LLC
Raphaël Santinelli, Nathalie Benz, Julie Guellec, Fabien Quinquis, Ervin Kocas, Johan Thomas, Tristan Montier, Chandran Ka, Emilie Luczka-Majérus, Edouard Sage,et al.
MDPI AG
Cystic Fibrosis (CF) is present due to mutations in the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) gene, the most frequent variant being p.phe508del. The CFTR protein is a chloride (Cl-) channel which is defective and almost absent of cell membranes when the p.Phe508del mutation is present. The p.Phe508del-CFTR protein is retained in the endoplasmic reticulum (ER) and together with inflammation and infection triggers the Unfolded Protein Response (UPR). During the UPR, the Activating Transcription Factor 6 (ATF6) is activated with cleavage and then decreases the expression of p.Phe508del-CFTR. We have previously shown that the inhibition of the activation of ATF6 alleviates the p.Phe508del-CFTR defects in cells overexpressing the mutated protein. In the present paper, our aim was to inhibit the cleavage of ATF6, and thus its activation in a human bronchial cell line with endogenous p.Phe508del-CFTR expression and in bronchial cells from patients, to be more relevant to CF. This was achieved by inhibiting the protease MBTP1 which is responsible for the cleavage of ATF6. We show here that this inhibition leads to increased mRNA and p.Phe508del-CFTR expression and, consequently, to increased Cl-efflux. We also explain the mechanisms linked to these increases with the modulation of genes when MBTP1 is inhibited. Indeed, RT-qPCR assays show that genes such as HSPA1B, CEBPB, VIMP, PFND2, MAPK8, XBP1, INSIG1, and CALR are modulated. In conclusion, we show that the inhibition of MBTP1 has a beneficial effect in relevant models to CF and that this is due to the modulation of genes involved in the disease.
Olivia Barada, Sophie Salomé-Desnoulez, Fahima Madouri, Gaëtan Deslée, Christelle Coraux, Philippe Gosset, and Muriel Pichavant
MDPI AG
Background: Dysregulated inflammation as seen in chronic obstructive pulmonary disease (COPD) is associated with impaired wound healing. IL-20 cytokines are known to be involved in wound healing processes. The purpose of this study was to use ex vivo and in vitro approaches mimicking COPD to evaluate the potential modulatory role of interleukin-20 (IL-20) on the inflammatory and healing responses to epithelial wounding. Methods: The expression of IL-20 cytokines and their receptors was investigated in lung-derived samples collected from non-COPD and COPD patients, from mice chronically exposed to cigarette smoke and from airway epithelial cells from humans and mice exposed in vitro to cigarette smoke. To investigate the role of IL-20 cytokines in wound healing, experiments were performed using a blocking anti-IL-20Rb antibody. Results: Of interest, IL-20 cytokines and their receptors were expressed in bronchial mucosa, especially on airway epithelial cells. Their expression correlated with the disease severity. Blocking these cytokines in a COPD context improved the repair processes after a lesion induced by scratching the epithelial layer. Conclusions: Collectively, this study highlights the implication of IL-20 cytokines in the repair of the airway epithelium and in the pathology of COPD. IL-20 subfamily cytokines might provide therapeutic benefit for patients with COPD to improve epithelial healing.
Anaëlle Muggeo, Christelle Coraux, and Thomas Guillard
Public Library of Science (PLoS)
Pseudomonas aeruginosa is a major, but opportunistic, respiratory pathogen, which rarely infects healthy individuals, mainly due to the barrier effect of the human airway epithelium (HAE). This review explores the interaction of P. aeruginosa with HAE and the progression of the infection. The basolateral part of the epithelium, which includes the basolateral membrane of the epithelial cells and the basement membrane, is inaccessible in normal tight epithelia with intact junctions. We highlight how P. aeruginosa exploits weaknesses in the HAE barrier to gain access to the basolateral part of the epithelium. This access is crucial to initiate respiratory infection and is mainly observed in the injured epithelium, in repairing or chronically remodeled epithelium, and during extrusion of senescent cells or cell multiplication during normal epithelium renewal. The subsequent adhesion of the bacteria and cytotoxic action of virulence factors, including the toxins delivered by the type 3 secretion system (T3SS), lead to retractions and cell death. Eventually, P. aeruginosa progressively reaches the basement membrane and propagates radially through the basal part of the epithelium to disseminate using twitching and flagellar motility.
L. Jahdauti, A. Muggeo, V. Paturel, S. Jaisson, E. Luczka, C. Coraux, and T. Guillard
Elsevier BV
Emilie Luczka-Majérus, Arnaud Bonnomet, Adeline Germain, Nathalie Lalun, Claire Kileztky, Jeanne-Marie Perotin, Gaëtan Deslée, Gonzague Delepine, Myriam Polette, Valérian Dormoy,et al.
European Respiratory Society (ERS)
COPD is characterised by a progressive and irreversible airflow limitation due to airway obstruction and emphysema [1]. We and others showed that bronchial epithelial remodelling in COPD is characterised by alteration of ciliogenesis and cilia function [2, 3], as well as a dysregulation of non-motile primary cilia (PC) [4]. In COPD, the main site of obstruction is in the small airways [5]. Considering that COPD is foremost a small airway disease (SAD) [6–8], we investigated the differentiation of bronchiolar epithelium in COPD, focusing on motile and primary ciliogenesis. An alteration of primary and motile ciliogenesis is detected in mild/moderate COPD small airways and could be at the origin of the initiation of epithelial remodelling http://bit.ly/3Tz3JDj
Antony Hoarau, Myriam Polette, and Christelle Coraux
MDPI AG
Hyaluronic acid (HA) is a major component of the extracellular matrix. It is synthesized by hyaluronan synthases (HAS) into high-molecular-weight chains (HMW-HA) that exhibit anti-inflammatory and immunomodulatory functions. In damaged, infected, and/or inflamed tissues, HMW-HA are degraded by hyaluronidases (HYAL) or reactive oxygen species (ROS) to give rise to low-molecular-weight HAs (LMW-HAs) that are potent pro-inflammatory molecules. Therefore, the size of HA regulates the balance of anti- or pro-inflammatory functions. The activities of HA depend also on its interactions with hyaladherins. HA synthesis, degradation, and activities through HA/receptors interactions define the hyaluronasome. In this review, a short overview of the role of high and low-molecular-weight HA polymers in the lungs is provided. The involvement of LMW-HA in pulmonary innate immunity via the activation of neutrophils, macrophages, dendritic cells, and epithelial cells is described to highlight LMW-HA as a therapeutic target in inflammatory respiratory diseases. Finally, the possibilities to counter LMW-HA’s deleterious effects in the lungs are discussed.
Frédéric Becq, Sandra Mirval, Thomas Carrez, Manuella Lévêque, Arnaud Billet, Christelle Coraux, Edouard Sage, and Anne Cantereau
European Respiratory Society (ERS)
Trikafta, currently the leading therapeutic in cystic fibrosis (CF), has demonstrated a real clinical benefit. This treatment is the triple combination therapy of two folding correctors elexacaftor/tezacaftor (VX445/VX661) plus the gating potentiator ivacaftor (VX770). In this study, our aim was to compare the properties of F508del-CFTR in cells treated with either lumacaftor (VX809), tezacaftor, elexacaftor, elexacaftor/tezacaftor with or without ivacaftor. We studied F508del-CFTR function, maturation and membrane localisation by Ussing chamber and whole-cell patch-clamp recordings, Western blot and immunolocalisation experiments. With human primary airway epithelial cells and the cell lines CFBE and BHK expressing F508del, we found that, whereas the combination elexacaftor/tezacaftor/ivacaftor was efficient in rescuing F508del-CFTR abnormal maturation, apical membrane location and function, the presence of ivacaftor limits these effects. The basal F508del-CFTR short-circuit current was significantly increased by elexacaftor/tezacaftor/ivacaftor and elexacaftor/tezacaftor compared to other correctors and nontreated cells, an effect dependent on ivacaftor and cAMP. These results suggest that the level of the basal F508del-CFTR current might be a marker for correction efficacy in CF cells. When cells were treated with ivacaftor combined to any correctors, the F508del-CFTR current was unresponsive to the subsequently acute addition of ivacaftor, unlike the CFTR (cystic fibrosis transmembrane conductance regulator) potentiators genistein and Cact-A1 which increased elexacaftor/tezacaftor/ivacaftor and elexacaftor/tezacaftor-corrected F508del-CFTR currents. These findings show that ivacaftor reduces the correction efficacy of Trikafta. Thus, combining elexacaftor/tezacaftor with a different potentiator might improve the therapeutic efficacy for treating CF patients.
Lionel Froux, Christelle Coraux, Edouard Sage, and Frédéric Becq
Springer Science and Business Media LLC
AbstractLoss-of-function mutations in the Cystic Fibrosis Transmembrane conductance Regulator (CFTR) channel in human airway epithelial cells are responsible for Cystic Fibrosis. A deleterious impact of physiological temperature on CFTR plasma membrane expression, residence and channel activity is characteristic of the most common and severe CF mutation, F508del. Using primary human F508del-airway epithelial cells and CF bronchial epithelial CFBE41o- cell lines expressing F508del- or WT-CFTR, we examined the effects of temperature (29 °C-39 °C) on the amplitude and stability of short-circuit CFTR-dependent currents over time and the efficiency of pharmacological strategies to stably restore F508del-CFTR function. We show that F508del-CFTR functional instability at 37 °C is not prevented by low temperature or VX-809 correction, genistein and VX-770 potentiators, nor by the combination VX-809/VX-770. Moreover, F508del-CFTR-dependent currents 30 minutes after CFTR activation at 37 °C did not significantly differ whether a potentiator was used or not. We demonstrate that F508del-CFTR function loss is aggravated at temperatures above 37 °C while limited by a small decrease of temperature and show that the more F508del-CFTR is stimulated, the faster the current loss happens. Our study highlights the existence of a temperature-dependent process inhibiting the function of F508del-CFTR, possibly explaining the low efficacy of pharmacological drugs in clinic.
Amal Kouadri, Mariam El Khatib, Johanna Cormenier, Sylvain Chauvet, Wael Zeinyeh, Micheline El Khoury, Laurence Macari, Pierre Richaud, Christelle Coraux, Isabelle Michaud-Soret,et al.
Mary Ann Liebert Inc
Aim: Bronchial epithelium acts as a defensive barrier against inhaled pollutants and microorganisms. This barrier is often compromised in inflammatory airway diseases that are characterized by excessive oxidative stress responses, leading to bronchial epithelial shedding, barrier failure, and increased bronchial epithelium permeability. Among proteins expressed in the junctional barrier and participating to the regulation of the response to oxidative and to environmental stresses is the cellular prion protein (PrPC). However, the role of PrPC is still unknown in the bronchial epithelium. Herein, we investigated the cellular mechanisms by which PrPC protein participates into the junctional complexes formation, regulation, and oxidative protection in human bronchial epithelium. Results: Both PrPC messenger RNA and mature protein were expressed in human epithelial bronchial cells. PrPC was localized in the apical domain and became lateral, at high degree of cell polarization, where it colocalized and interacted with adherens (E-cadherin/γ-catenin) and desmosomal (desmoglein/desmoplakin) junctional proteins. No interaction was detected with tight junction proteins. Disruption of such interactions induced the loss of the epithelial barrier. Moreover, we demonstrated that PrPC protection against copper-associated oxidative stress was involved in multiple processes, including the stability of adherens and desmosomal junctional proteins. Innovation: PrPC is a pivotal protein in the protection against oxidative stress that is associated with the degradation of adherens and desmosomal junctional proteins. Conclusion: Altogether, these results demonstrate that the loss of the integrity of the epithelial barrier by oxidative stress is attenuated by the activation of PrPC expression, where deregulation might be associated with respiratory diseases.
Antoine Guillon, Deborah Brea, Emilie Luczka, Virginie Hervé, Soujoud Hasanat, Camille Thorey, Magdiel Pérez-Cruz, Juliette Hordeaux, Julie Mankikian, Philippe Gosset,et al.
Elsevier BV
Jeanne-Marie Perotin, Christelle Coraux, Eymeric Lagonotte, Philippe Birembaut, Gonzague Delepine, Myriam Polette, Gaëtan Deslée, and Valérian Dormoy
European Respiratory Society (ERS)
Chronic obstructive pulmonary disease (COPD) is a major economic and social concern worldwide because of its impact on mortality and morbidity [1]. COPD is characterised by airway epithelium remodelling, a hallmark of dysregulated airway epithelium plasticity [2]. There are currently no available therapeutics to restore the integrity and functionality of the epithelium. Therefore, novel sources of investigation are becoming crucial to understand the alterations at the root of COPD initiation. Non-motile primary cilia are solitary sensor organelles playing a critical role in cell cycle control, proliferation, polarity and differentiation, particularly of ciliated cells possessing motile cilia [3, 4]. Primary cilia are assembled on different types of human cells depending on their state and activities in response to cellular quiescence where they relay extracellular signals and retract upon cell cycle re-entry [5]. Alterations of primary cilium structure and function are responsible for ciliopathies [6, 7]. Primary cilia may be crucial in determining outcomes during airway epithelial cell differentiation thus we hypothesised that primary cilia are present in adult epithelial cells and may play a key role in airway plasticity. First, we investigated the presence and localisation of primary cilia in the bronchial epithelium. Secondly, we analysed the relationships between primary cilia and clinical, functional and histological characteristics of non-COPD and COPD patients. Non-differentiated airway epithelial cells display primary cilia and their number is associated with COPD features http://ow.ly/wiGH30jDbeG
Florence Sonneville, Manon Ruffin, Christelle Coraux, Nathalie Rousselet, Philippe Le Rouzic, Sabine Blouquit-Laye, Harriet Corvol, and Olivier Tabary
Springer Science and Business Media LLC
Marie-Laure Calvez, Nathalie Benz, Florentin Huguet, Aude Saint-Pierre, Elise Rouillé, Christelle Coraux, Claude Férec, Mathieu Kerbiriou, and Pascal Trouvé
Public Library of Science (PLoS)
Cystic fibrosis (CF) is the most common autosomal recessive disease in Caucasians caused by mutations in the gene encoding the Cystic Fibrosis Transmembrane conductance Regulator (CFTR) chloride (Cl-) channel regulated by protein kinases, phosphatases, divalent cations and by protein-protein interactions. Among protein-protein interactions, we previously showed that Annexin A5 (AnxA5) binds to CFTR and is involved in the channel localization within membranes and in its Cl- channel function. The deletion of phenylalanine at position 508 (F508del) is the most common mutation in CF which leads to an altered protein (F508del-CFTR) folding with a nascent protein retained within the ER and is quickly degraded. We previously showed that AnxA5 binds to F508del-CFTR and that its increased expression due to a Gonadoliberin (GnRH) augments Cl- efflux in cells expressing F508del-CFTR. The aim of the present work was to use the GnRH analog buserelin which is already used in medicine. Human nasal epithelial cells from controls and CF patients (F508del/F508del) were treated with buserelin and we show here that the treatment alleviates Cl- channel defects in CF cells. Using proteomics we highlighted some proteins explaining this result. Finally, we propose that buserelin is a potential new pharmaceutical compound that can be used in CF and that bronchus can be targeted since we show here that they express GnRH-R.
Arnaud Bonnomet, Emilie Luczka, Christelle Coraux, and Ludovic de Gabory
Wiley
The regulation of mucociliary clearance is a key part of the defense mechanisms developed by the airway epithelium. If a high aggregate quality of evidence shows the clinical effectiveness of nasal irrigation, there is a lack of studies showing the intrinsic role of the different irrigation solutions allowing such results. This study investigated the impact of solutions with different pH and ionic compositions, eg, normal saline, non‐diluted seawater and diluted seawater, on nasal mucosa functional parameters.
Clémence O. Henry, Emilie Dalloneau, Maria-Teresa Pérez-Berezo, Cristina Plata, Yongzheng Wu, Antoine Guillon, Eric Morello, Rose-France Aimar, Marie Potier-Cartereau, Frédéric Esnard,et al.
American Physiological Society
Cystic fibrosis (CF) is an inherited disease associated with chronic severe lung inflammation, leading to premature death. To develop innovative anti-inflammatory treatments, we need to characterize new cellular and molecular components contributing to the mechanisms of lung inflammation. Here, we focused on the potential role of “transient receptor potential vanilloid-4” (TRPV4), a nonselective calcium channel. We used both in vitro and in vivo approaches to demonstrate that TRPV4 expressed in airway epithelial cells triggers the secretion of major proinflammatory mediators such as chemokines and biologically active lipids, as well as a neutrophil recruitment in lung tissues. We characterized the contribution of cytosolic phospholipase A2, MAPKs, and NF-κB in TRPV4-dependent signaling. We also showed that 5,6-, 8,9-, 11,12-, and 14,15-epoxyeicosatrienoic acids, i.e., four natural lipid-based TRPV4 agonists, are present in expectorations of CF patients. Also, TRPV4-induced calcium mobilization and inflammatory responses were enhanced in cystic fibrosis transmembrane conductance regulator-deficient cellular and animal models, suggesting that TRPV4 is a promising target for the development of new anti-inflammatory treatments for diseases such as CF.
Damien Adam, Jacqueline Roux-Delrieu, Emilie Luczka, Arnaud Bonnomet, Julien Lesage, Jean-Claude Mérol, Myriam Polette, Michel Abély, and Christelle Coraux
Wiley
Chronic inflammation is a hallmark of cystic fibrosis (CF) lung disease and airway epithelium damage and remodelling are important components of lung pathology progression in CF. Whether this remodelling is secondary to deleterious infectious and inflammatory mediators, or to alterations of CF human airway epithelial (HAE) cells, such as their hyper inflammatory phenotype or their basic cystic fibrosis transmembrane conductance regulator (CFTR) default, remains debated. In this study, we evaluated the involvement of alterations of CF HAE cells in airway epithelium remodelling. HAE cells from non‐CF and CF patients were cultured in an air–liquid interface, with and without inflammatory stimulation, along the regeneration process, and the remodelling of the reconstituted epithelium was analysed. We confirmed that CF HAE cells showed a hyperinflammatory phenotype which was lost with time. In comparison to non‐CF epithelium, CF epithelium regeneration in the absence of exogenous inflammation was higher and exhibited basal cell hyperplasia. This remodelling was mimicked by inflammatory stimulation of non‐CF cells and was absent when CF HAE cells were no longer hyperinflamed. Moreover, the number of goblet cells was similar in non‐CF and CF cultures and increased equally under inflammatory stimulation. Finally, whatever the inflammatory environment, CF cultures showed a delay in ciliated cell differentiation. In conclusion, alterations of CF HAE cells partly regulate airway epithelium remodelling following injury and regeneration. This remodelling, together with goblet cell hyperplasia induced by exogenous inflammation and alteration of ciliated cell differentiation, may worsen mucociliary clearance impairment, leading to injury. Copyright © 2014 Pathological Society of Great Britain and Ireland. Published by John Wiley & Sons, Ltd.
Jeanne-Marie Perotin, Damien Adam, Juliette Vella-Boucaud, Gonzague Delepine, Sebastian Sandu, Anne-Carole Jonvel, Alain Prevost, Gérard Berthiot, Christophe Pison, François Lebargy,et al.
Springer Science and Business Media LLC
D. Adam, J.-M. Perotin, F. Lebargy, P. Birembaut, G. Deslée, and C. Coraux
Elsevier BV
Kamel Maouche, Kahina Medjber, Jean-Marie Zahm, Franck Delavoie, Christine Terryn, Christelle Coraux, Stéphanie Pons, Isabelle Cloëz-Tayarani, Uwe Maskos, Philippe Birembaut,et al.
Proceedings of the National Academy of Sciences
Loss or dysfunction of the cystic fibrosis (CF) transmembrane conductance regulator (CFTR) leads to impairment of airway mucus transport and to chronic lung diseases resulting in progressive respiratory failure. Nicotinic acetylcholine receptors (nAChRs) bind nicotine and nicotine-derived nitrosamines and thus mediate many of the tobacco-related deleterious effects in the lung. Here we identify α7 nAChR as a key regulator of CFTR in the airways. The airway epithelium in α7 knockout mice is characterized by a higher transepithelial potential difference, an increase of amiloride-sensitive apical Na + absorption, a defective cAMP-dependent Cl − conductance, higher concentrations of Na + , Cl − , K + , and Ca 2+ in secretions, and a decreased mucus transport, all relevant to a deficient CFTR activity. Moreover, prolonged nicotine exposure mimics the absence of α7 nAChR in mice or its inactivation in vitro in human airway epithelial cell cultures. The functional coupling of α7 nAChR to CFTR occurs through Ca 2+ entry and activation of adenylyl cyclases, protein kinase A, and PKC. α7 nAChR, CFTR, and adenylyl cyclase-1 are physically and functionally associated in a macromolecular complex within lipid rafts at the apical membrane of surface and glandular airway epithelium. This study establishes the potential role of α7 nAChR in the regulation of CFTR function and in the pathogenesis of smoking-related chronic lung diseases.
Nguyen Thu Ngan Trinh, Olivier Bardou, Anik Privé, Emilie Maillé, Damien Adam, Sarah Lingée, Pasquale Ferraro, Martin-Yvon Desrosiers, Christelle Coraux, and Emmanuelle Brochiero
European Respiratory Society (ERS)
Airway damage and remodelling are important components of lung pathology progression in cystic fibrosis (CF). Although repair mechanisms are engaged to restore the epithelial integrity, these processes are obviously insufficient to maintain lung function in CF airways. Our aims were therefore to study how the basic cystic fibrosis transmembrane conductance regulator (CFTR) defect could impact epithelial wound healing and to determine if CFTR correction could improve it. Wound-healing experiments, as well as cell migration and proliferation assays, were performed to study the early phases of epithelial repair in human CF and non-CF airway cells. CFTR function was evaluated using CFTR small interferring (si)RNA and inhibitor GlyH101 in non-CF cells, and conversely after CFTR rescue with the CFTR corrector VRT-325 in CF cells. Wound-healing experiments first showed that airway cells from CF patients repaired slower than non-CF cells. CFTR inhibition or silencing in non-CF primary airway cells significantly inhibited wound closure. GlyH101 also decreased cell migration and proliferation. Interestingly, wild-type CFTR transduction in CF airway cell lines or CFTR correction with VRT-325 in CFBE-&Dgr;F508 and primary CF bronchial monolayers significantly improved wound healing. Altogether our results demonstrated that functional CFTR plays a critical role in wound repair, and CFTR correction may represent a novel strategy to promote the airway repair processes in CF.
Nihal Engin Vrana, Agnes Dupret-Bories, Charlotte Bach, Christophe Chaubaroux, Christelle Coraux, Dominique Vautier, Fouzia Boulmedais, Youssef Haikel, Christian Debry, Marie-Helene Metz-Boutigue,et al.
Wiley
Previously, we showed that macroporous titanium implants, colonized in vivo together with an epithelial graft, are viable options for tracheal replacement in sheep. To decrease the number of operating steps, biomaterial‐based replacements for epithelial graft and intramuscular implantation were developed in the present study. Hybrid microporous PLLA/titanium tracheal implants were designed to decrease initial stenosis and provide a surface for epithelialization. They have been implanted in New Zealand white rabbits as tracheal substitutes and compared to intramuscular implantation samples. Moreover, a basement membrane like coating of the implant surface was also designed by Layer‐by‐Layer (LbL) method with collagen and alginate. The results showed that the commencement of stenosis can be prevented by the microporous PLLA. For determination of the optimum time point of epithelialization after implantation, HPLC analysis of blood samples, C‐reactive protein (CRP), and Chromogranin A (CGA) analyses and histology were carried out. Following 3 weeks the implant would be ready for epithelialization with respect to the amount of tissue integration. Calcein‐AM labeled epithelial cell seeding showed that after 3 weeks implant surfaces were suitable for their attachment. CRP readings were steady after an initial rise in the first week. Cross‐linked collagen/alginate structures show nanofibrillarity and they form uniform films over the implant surfaces without damaging the microporosity of the PLLA body. Human respiratory epithelial cells proliferated and migrated on these surfaces which provided a better alternative to PLLA film surface. In conclusion, collagen/alginate LbL coated hybrid PLLA/titanium implants are viable options for tracheal replacement, together with in situ epithelialization. Biotechnol. Bioeng. 2012; 109:2134–2146. © 2012 Wiley Periodicals, Inc.
Lisa Giovannini-Chami, Nathalie Grandvaux, Laure-Emmanuelle Zaragosi, Karine Robbe-Sermesant, Brice Marcet, Bruno Cardinaud, Christelle Coraux, Yves Berthiaume, Rainer Waldmann, Bernard Mari,et al.
Humana Press
Jean-Marie Zahm, Magali Milliot, Anthony Bresin, Christelle Coraux, and Philippe Birembaut
Elsevier BV
Brice Marcet, Benoît Chevalier, Christelle Coraux, Laurent Kodjabachian, and Pascal Barbry
Informa UK Limited
Multiciliated cells lining the surface of some vertebrate epithelia are essential for various physiological processes, such as airway cleansing. Their apical surface is constituted by hundreds of motile cilia, which beat in a coordinated manner to generate directional fluid flow. We recently reported the identification of microRNAs of the miR-449 family as evolutionary conserved key regulators of vertebrate multiciliogenesis. This novel function of miR-449 was established using in vivo and in vitro antisense approaches in two distinct experimental models. miR-449 strongly accumulated in multiciliated cells in human airway epithelium and Xenopus laevis embryonic epidermis, where it triggered centriole multiplication and multiciliogenesis by directly repressing the Delta/Notch pathway. Our data complement previous reports that showed the blocking action of miR-449 on the cell cycle, and unraveled a novel conserved mechanism whereby Notch signaling must undergo microRNA-mediated inhibition to permit differentiation of ciliated cell progenitors. We review here several important questions regarding the links between microRNAs and the Notch pathway in the control of cell fate.